Stakeholders in the health sector have called for a renewed political commitment, increased investment in the workforce, and clearer policy reforms to strengthen maternal healthcare services across Nigeria.
They made the call on Tuesday at the 2025 Task-Shifting Symposium in Abuja, themed “Bridging research, policy, and practice for better maternal healthcare in Nigeria.”
Speaking at the event, the Mandate Secretary of the Federal Capital Territory Administration (FCTA) Health Services and Environment Secretariat, Adedolapo Fasawe, said task shifting, which involves delegating specific responsibilities from highly specialised professionals to trained lower-cadre health workers, remains vital for expanding access to maternal care.
Ms Fasawe, however, warned that its success depends on clear protocols, structured supervision, continuous training, and strict adherence to evidence-based practice.
She noted that primary health research is crucial for understanding systemic barriers, designing context-sensitive interventions, and informing policy to promote accountability and continuous improvement.
“Task shifting has been globally recognised as a practical and effective strategy for expanding access to essential maternal healthcare. This means redistributing certain tasks from more specialised professionals to well-trained and supervised less specialised cadres,” she said.
“When implemented well, task shifting has been shown to reduce delays in emergency obstetric care, expand access to life-saving interventions, improve continuity of antenatal and postnatal care, and reduce the workload of overstretched skilled birth attendants.”
Citing examples from Ethiopia and Uganda, Ms Fasawe noted that countries adopting well-structured task-shifting models have recorded improvements in skilled birth attendance and decreases in preventable maternal deaths.
Importance of research
Ms Fasawe highlighted the central role of research in shaping meaningful policy.
She added that primary health research plays three critical roles in improving maternal healthcare.
“Research helps us understand systemic barriers, guides context-sensitive interventions, and supports accountability and continuous improvement,” she said.
“Evidence tells us what needs refining, what needs scaling, and what needs to be discontinued. This is how research becomes the bridge between vision and impact. Policy becomes truly effective only when it is constantly informed by frontline evidence.”
She reaffirmed the FCT’s commitment to reducing preventable maternal and child deaths.
“We have zero tolerance for maternal, infant, or neonatal mortality in the FCT. We always say there’s no reason for a woman to die while bringing life into the world,” she said.
Maternal mortality
Nigeria has some of the highest cases of maternal mortality, with 1,047 deaths per 100,000 live births, according to the World Health Organisation (WHO).
In a report titled “Improving Maternal and Newborn Health and Survival and Reducing Stillbirths: Progress Report 2023,” WHO revealed that Nigeria ranked second behind India in maternal and neonatal deaths, with 82,000 maternal deaths, 181,000 stillbirths, and 277,000 neonatal deaths.
The country’s 540,000 deaths represent 12 per cent of global maternal, stillbirth, and neonatal deaths, despite contributing just six per cent of the world’s live births.
This data reflects both Nigeria’s large population and the deep gaps in its health system.
Workforce shortages undermining maternal care
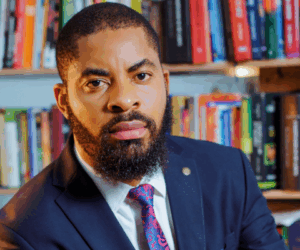
Public Health Physician and Honorary Postdoctoral Researcher at the University of Oxford’s Nuffield Department of Primary Care Health Sciences, Francis Ayomoh, stressed the need for stronger government action to address severe workforce shortages in primary healthcare facilities.
Presenting findings from his study, “Task-Shifting for Maternal Healthcare Services: A Qualitative Study of Policy and Practice in Nigeria’s Primary Healthcare System,” Mr Ayomoh said Nigeria remains one of the world’s largest contributors to maternal deaths and that the workforce crisis makes task shifting unavoidable.
“The findings suggest that at least 50 per cent of primary healthcare workers in the FCT are unpaid volunteers who rely on stipends from facilities rather than government salaries,” he said.
“This precarious situation requires urgent attention. One key recommendation is increased government funding to employ more PHC workers.”
He added that many trained community health workers, nurses, and midwives remain unemployed despite the shortage.
“It is no news that we have a severe health workforce shortage. This is why task shifting was necessary. But the study we conducted has shed more light on what the issues are with task shifting,” he noted.
READ ALSO: Nigerian govt pushes gender-inclusive policies to empower women, children, others
He explained that the main challenge is balancing access to maternal healthcare with maintaining service quality, given the significant human resource gap.
Mr Ayomoh called for continuous training, supportive supervision, and greater investment in patient-centred care, adding that “Let’s employ as many as the government can afford to pay.”