The fight for a child’s life in Katsina State does not begin in a hospital bed; it sometimes begins on the road. By the time Aisha Rabe reached Katsina city from Sandamu, the midday sun had turned the air into a suffocating wall of heat.
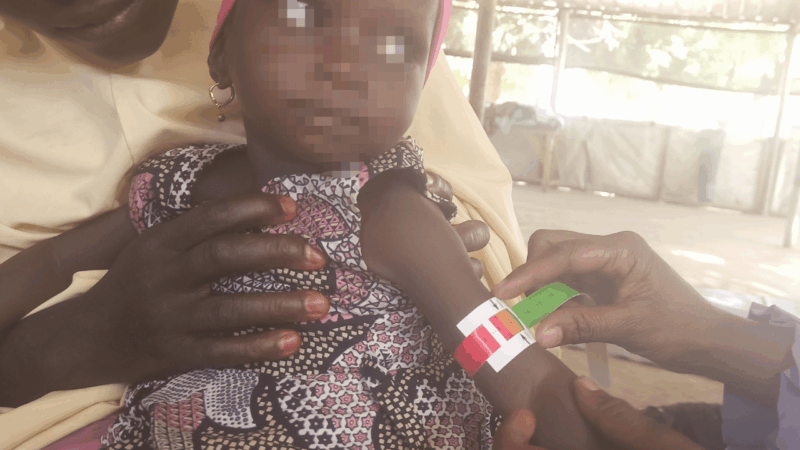
Her five-month-old daughter lay limp against her chest, having gone two days without suckling. Fever had sapped every ounce of energy from her tiny body, and she had grown worryingly light in Mrs Rabe’s arms, signs that point to severe malnutrition.

Inside the Inpatient Therapeutic Feeding Centre (ITFC) at the Turai Umaru Yar’Adua Maternity and Children’s Hospital, the nurses barely glanced up as Mrs Rabe stumbled in. They were already running between beds, attending to children whose survival hung by a thread.
The ward was overflowing. Missing beds had been replaced with mats on the floor, where mothers crouched beside frail infants, their tiny chests rising and falling with each laboured breath.
This chaotic, tense space marks the ‘survival line’, the first 48 to 96 hours when a child must respond to treatment, or risk slipping beyond the reach of medicine.
Inside the Ward Where Time is the Enemy
Mrs Rabe’s struggle is part of a much larger emergency. The 2024 hunger season pushed Katsina’s emergency nutrition system beyond anything it had seen before. Nearly 10,000 critically malnourished children cycled through the stabilisation system at its peak.
Across northern Nigeria, the humanitarian organisation Médecins Sans Frontières (MSF) reported that its outpatient units recorded almost 300,000 admissions—more than half of the organisation’s global caseload that year.
As of July, MSF said over 650 children had died from severe acute malnutrition in Katsina State in 2025 alone.
The organisation said the number of children suffering from nutritional oedema — the most severe and life-threatening form of malnutrition in Katsina State — had surged by more than 200 per cent compared with the same period last year.

This scale of crisis translates to a national loss estimated at $56 billion in human capital annually, according to Vice President Kashim Shettima.
Inside the ward, those numbers became faces. Every nurse knew the hard truth: more sick children were arriving than the facility could hold.
Najib Badamasi, a nutrition assistant at the Inpatient Therapeutic Feeding Centre, explained the routine with painful precision.
“Two to four days. That’s the maximum for initial stabilisation. We can’t keep them longer. More children are coming,” Mr Badamasi said.
Sola Abidurrahman, a medical doctor at the centre, also noted that “Our work is not to keep them till they are fully recovered. It is to prevent death.”

The ward moved like a place caught between a crisis and a race against time. Nurses threaded cannulas into twig-thin arms, administered F-75 and F-100 therapeutic milk, and attempted to coax life back into bodies running out of time.
The heat, the coughing, the wailing, the exhaustion—it all blended into a single atmosphere of urgency.
And yet, the success rate is astonishing: 90 per cent of children stabilise within the first 48 hours. But “stabilise” in this ward does not mean “safe.” It means “alive—for now.”
Aisha’s five days
For children like Mrs Rabe’s daughter, crossing the “survival line” was a test of both medicine and luck.
When Mrs Rabe arrived, her daughter was too weak to swallow food. The nurses inserted a feeding tube, crushed medications into tiny doses, and wrapped her trembling body in layers of cloth to fight the cold that often accompanies severe malnutrition.
Her breaths were shallow, and her eyes could barely focus. Her weight, dangerously low, told its own story.
For the first two days, nothing changed. Mrs Rabe hardly moved from the edge of the mat, watching her daughter’s chest rise and fall in uneven rhythms.
Every sound in the ward, the wail of another child, the call for a nurse, made her flinch.
She had been told that these first days were when decisions of life and death happen quietly, almost invisibly.
Then, on the fifth day, the shift came. Mrs Rabe leaned close and whispered a sentence that felt almost unreal: “She has started suckling, fine.”
It was the first sign that the child’s body was responding and that she might cross the threshold the nurses call stabilisation.
But even her relief carried a shadow. The full stay in the stabilisation centre would last roughly two weeks—after which she would be discharged, still weak, still fragile, and still returning to the same conditions that nearly killed her.
The staff could not keep them longer because another child would need that bed. Another mother would step through the doors with hope stitched to despair.
For the family of one-year-old Bilkisu, who arrived at the centre so weak that “she couldn’t even suckle when we came,” the short stay was a frightening blur.
Though medically stabilised, the family was forced to manage the long-term journey of recovery alone, stepping out of the relative safety of the clinic and back into an environment of extreme scarcity.
Malnutrition crisis in Nigeria
According to the United Nations Children’s Fund (UNICEF), about two million Nigerian children suffer from severe acute malnutrition (SAM), but only one in five receive treatment. Seven per cent of women of childbearing age also suffer from acute malnutrition.
SAM is a serious condition where children do not get enough nutrients and energy to grow and develop properly. It can lead to weakened immunity, making children more vulnerable to infections and even death if untreated.
The crisis in Katsina is a reflection of a broader regional emergency; however, recent data specific to the state reveal the terrifying scale of the problem. While the 2024 Nigeria Demographic and Health Survey (NDHS) confirms that the North-west zone bears the heaviest burden of child mortality in the country, state-specific findings presented at the recent High-Level Conference are even more alarming.
According to the 2024 North-west Nutrition Survey, presented by the North-west Governors Forum, malnutrition in Katsina has reached critical levels. The survey revealed that 11.6 per cent of children under five in Katsina State suffer from acute malnutrition, a life-threatening condition requiring immediate treatment.
Even more concerning is the long-term impact: the survey disclosed that in Katsina, “half of all children are stunted”—too short for their age, too undernourished to learn, and too weak to thrive.
This data validates the urgent warnings from medical staff on the ground; for children in Katsina, malnutrition is not just a health shock, but a generational crisis.
Poverty, conflict and chaos
The pressure that forces a frantic 48-hour turnover inside Katsina’s stabilisation wards does not start in the hospital. It begins much earlier inside homes stretched to breaking point by poverty, insecurity, and a collapsing rural economy.
These overlapping crises guarantee a steady stream of children arriving at the very edge of survival.
In many communities, the math of daily life is brutally simple: too many dependents, too few resources. One mother’s story revealed just how deep the problem runs.
Her husband works as a casual labourer, taking whatever jobs appear—building work, loading trucks, or farm tasks in another town. His income can double today and disappear tomorrow. What never changes are the responsibilities waiting at home: two wives, ten children, and a household where food decisions are made one day at a time.
Six of the children are under five, the most vulnerable to acute malnutrition. Their mother revealed that all six had been hospitalised for malnutrition within the last 12 months. She said this quietly, not out of shame, but fatigue.
The family eats twice a day, on the days they can afford to do so. Their savings rarely exceed N10,000, an amount that can be wiped out in a single medical emergency.
“When it finishes,” the mother said, “We go to beg those whom God has blessed.”
Her words echo a reality that stretches far beyond her home. The roots of Katsina’s malnutrition crisis lie not only in medical wards but also in villages where hunger has become a routine, where insecurity prevents farmers from accessing their land, and where rising prices make survival a daily calculation.
In many of these households, child malnutrition is not the disease. It is the symptom of structural hunger, economic fragility, and a social system left to absorb shocks it cannot bear.
Triple threat of neglect
But poverty alone does not explain why so many children end up at death’s edge. Three forces: violence, climate shocks, and institutional neglect, work together to push families past breaking point.
The treatment journey is often the first barrier. The roads leading to the nutrition clinic are mined with fear. Bandits patrol these routes, making the journey a trauma where caregivers are stopped and warned to be “very quick to collect the Ready to Use Therapeutic Food (RUTF) and go back home.” If not, they would definitely punish them.
Furthermore, the cost of accessing care is often consumed by transportation: “We received some caregivers… they said it cost almost N7,000 to get here,” Ms Badamasi, the nutritional assistant, confirmed.
The crisis is guaranteed to worsen due to environmental collapse: recent rainy season floods have resulted in a predicted food crisis, with farmers in Kaita and Jibia reporting that essential crops like rice and millet were “covered” by floodwaters.
Yet, in the wake of this devastation, mothers confirmed that no government aid or inspection had reached their community to assess the damage.
Government’s policy pivot
Faced with these overwhelming numbers and criticism from international bodies like MSF, the Katsina State Government insists it is no longer looking the other way.
The severe challenges, specifically the lack of funding, insufficient coverage, and systemic poverty, are being directly addressed by the state’s leadership, officials said.
Shamsudeen Yahaya, executive secretary of the Katsina Primary Healthcare Development Agency, characterised the MSF report as a “wake-up call” that catalysed a major policy pivot.
“Contrary to what people expected that government is going to deny, you know, about the figures, we took it as a wake-up call,” Mr Yahaya stated.
Addressing coverage and infrastructure gaps, Mr Yahaya said the state is moving decisively to address the clinical capacity issues that have led to the 48-hour discharge line.
He added that the Governor of Katsina State, Dikko Radda, approved the establishment of 60 new OTP (Outpatient Therapeutic Point) sites, five per LGA, and the revitalisation of the nine existing state-managed stabilisation centres.

Crucially, Mr Yahaya said this physical expansion is backed by a massive financial injection. Governor Radda announced that the state has invested over N14 billion in the health sector in 2024.
This includes a N1 billion contribution to the Child Nutrition Fund in partnership with UNICEF (2023-2025), N500 million approved specifically for the immediate procurement of RUTF, and an additional N700 million for the ARRIN 2 project.
To simultaneously combat poverty, the governor approved the distribution of 90 bags (each weighing 100kg) of assorted grains to 40,000 identified malnourished children and 90,000 vulnerable households.
To ensure sustainability at the local level, routine support to LGAs for nutrition was quadrupled from N250,000 to N1 million per LGA per month.
Fixing the “Payroll Paradox” and Accountability
The government’s response also directly confronts the systemic operational challenges raised by NGO staff, particularly the “Payroll Paradox”, a situation where state-owned facilities effectively rely on NGO-funded staff to function, masking workforce shortages.
Addressing the shortages that forced facilities to operate with six nurses instead of the required ten, Mr Yahaya highlighted that while recruitment for 1,020 permanent PHC staff is ongoing, the immediate financial commitment is designed to make the system more robust.
Additionally, Governor Radda has pledged to consider approving six months of maternity leave for nursing mothers to aid in exclusive breastfeeding. He also revealed plans for the sustainable, local production of RUTF and Tom-Brown factories.
Simultaneously, the state is tackling the “diversion” of supplies—a vulnerability where caregivers might sell RUTF or induce illness to secure more rations. To combat this, Mr Yahaya said strict accountability measures are being introduced, including biometric tracking and the establishment of mobile courts to try individuals responsible for misuse.
Finally, the approach to data has reportedly shifted. Mr Yahaya said that a comprehensive survey covering all 34 LGAs indicated “remarkable improvement” in the malnutrition trend compared to the previous year.
READ ALSO: SPECIAL REPORT: How conflict is driving child malnutrition in Benue
Beyond the emergency ward
The medical teams in Katsina perform a miracle every day, pulling fragile lives back from death’s door in a rapid, 48-hour sequence. This heroic, efficient response is the survival line that prevents a full collapse.
Now, that critical line is being supported by an unprecedented mobilisation from the state government, international partners like the EU (pledging £10 million), and federal leadership. Vice President Shettima’s warning serves as a final, urgent directive: “The child in Dutsin-Ma, the mother in Jibia, the family in Funtua—they cannot afford our delays.”
The battle is no longer fought only in the emergency ward, but also in the policy offices, the remote LGAs, and the fields. The initial race for life has led to a much-needed long-term race for livelihood.
The children may be stabilised, but their long-term survival now depends on the seamless integration of this new structural commitment with the clinical dedication that held the line for 48 hours.
Ultimately, success will be measured when the survival of a child in Katsina no longer depends on a frantic 48-hour race, but on a system that protects them before the fever begins.
This reporting was completed with the support of the Centre for Journalism Innovation and Development (CJID).